Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF)
Transforaminal Lumbar Interbody Fusion (TLIF) is a procedure used to fuse the lumbar spine via an approach from the back of the spine. The abbreviation TLIF stands for:
Transforaminal - The spine and intervertebral disc is accessed on one side only by removing the facet joint on the symptomatic side. The lumbar spine is accessed via a surgical approach from the behind through one or two small incisions in the lower part of your lumbar region.
Lumbar - one or more vertebrae (bones) of the lumbar spine are fused.
Interbody - fusion occurs between the two vertebral bodies following removal of the intervertebral disc. The fusion occurs accross the disc space.
Fusion - formation of bony bridge between segments of the spine in order to stablise the spine
Video - MIS TLIF Spinal Fusion Explainer Video
Video Courtesy of Nebula Health
|
TLIF surgery is generally used to treat leg pain (sciatica) and back pain, most commonly caused by degenerative disc disease and subsequent pressure on the lumbar nerves. Common reasons why TLIF surgery might be recommended over simpler decompressive spinal procedures (such as laminectomy and lumbar decompression) which don't fuse the spine include:
|
Image demonstrating:
a) Removal of the facet joint on one side to decompress the nerves b) Insertion of pedicle screws connected to rods to fuse the spine 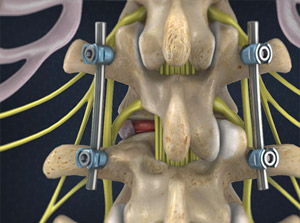 |
During TLIF surgery, Dr Oehme will stabilise the spine by fusing two or more vertebrae together with bone graft material. The procedure generally incorporates an extensive lumbar decompression and facetectomy on the symptomatic side, and the disc between the vertebral bodies is almost totallly removed. An interbody spacer called a cage, designed to promote fusion and restore spinal alignment, is implanted into the interbertebral space. Fusing the spine aims to improve symptoms of back pain related to degenerative disc disease and instability. The spinal segment to be fused is generally immobilised by the insertion of a rigid metal construct, such as pedicle screws connected to rods.
The TLIF procedure allows for a substantial lumbar nerve decompression curing symptoms related to disc herniation and lumbar stenosis. The pressure on the nerves is relieved eliminating symptoms of leg pain and sciatica, neurogenic claudication and radiculopathy. Walking and exercise tolerance is improved. Approaching the spine from the back allows for careful and direct decompression of the nerves. Using minimally invasive techniques and extensive decompression of the nerves can be performed through a small incision.
Dr Oehme performs TLIF surgery using minimally invasive and keyhole techniques. Patients typically have two small incisions in their lumbar spine which are 3-4cm in length and have absorbable sutures, which don't need to be removed. Patients are typically in hospital for between two and five days. Post opreative pain is generally easily managed with oral medications.
For more information about TLIF surgery watch the video below.
Video - MIS TLIF Spinal Fusion
Performing TLIF surgery using minimally invasive and keyhole techniques benefits patients by
Dr Oehme routinely uses advanced spinal neuronavigation equipment for accurate pedicle screw and instrumentation placement during fusion surgery. He has access to O-arm neuronavigation and other sophisticated neuronavigation technology which minimises the chance of a complication occurring. Dr Oehme also routinely uses intra-operative neural monitoring to minimise the possibility of nerve damage occurring.
It is against Dr Oehme's priniciple of harm minimisation to unneccessarily take iliac crest bone graft from your hip in order to promote fusion. Where possible, Dr Oehme uses synthetic bone substitutes and local bone so that complications of chronic hip pain do not occur.
Dr Oehme will advise if a MIS TLIF procedure is appropriate for your spinal condition. For more information or to arrange a time to discuss surgery with Dr Oehme contact Keyhole Neurosurgery on 1800 DO SPINE (1800 367 746).
- minimising muscle injury
- reducing blood loss
- reducing infection risk
- reducing postoperative pain
- shortening the time spent in hospital
- utilising smaller more cosmetically favourable incisions
- reducing damage to adjacent levels
Dr Oehme routinely uses advanced spinal neuronavigation equipment for accurate pedicle screw and instrumentation placement during fusion surgery. He has access to O-arm neuronavigation and other sophisticated neuronavigation technology which minimises the chance of a complication occurring. Dr Oehme also routinely uses intra-operative neural monitoring to minimise the possibility of nerve damage occurring.
It is against Dr Oehme's priniciple of harm minimisation to unneccessarily take iliac crest bone graft from your hip in order to promote fusion. Where possible, Dr Oehme uses synthetic bone substitutes and local bone so that complications of chronic hip pain do not occur.
Dr Oehme will advise if a MIS TLIF procedure is appropriate for your spinal condition. For more information or to arrange a time to discuss surgery with Dr Oehme contact Keyhole Neurosurgery on 1800 DO SPINE (1800 367 746).
Risks of MIS TLIF
Most TLIF surgeries can be performed safely without any complications. However, like any surgical procedure there are risks associated with both the anaesthetic and the procedure itself.
Risks of Anaesthesia
Risks of anaesthesia will be discussed with you by your anaesthetist prior to surgery. It is important that you inform us of your correct age and any past medical problems, as this can influence the risk of anaesthesia. Risks include:
General Risks of Spine Surgery
Although spine surgery is generally safe, there are some risks whenever operations on the spine are performed. These include:
Specific Risks of Transforaminal Lumbar Interbody Fusion
The specific risks will be discussed in detail prior to your surgery but may include:
Most TLIF surgeries can be performed safely without any complications. However, like any surgical procedure there are risks associated with both the anaesthetic and the procedure itself.
Risks of Anaesthesia
Risks of anaesthesia will be discussed with you by your anaesthetist prior to surgery. It is important that you inform us of your correct age and any past medical problems, as this can influence the risk of anaesthesia. Risks include:
- Heart problems, such as heart attack (AMI) or arrhythmia
- Lung problems, such as infection (pneumonia) or blood clots
- Urinary tract infection
- Deep Venous Thrombosis (DVT)
- Eye or visual problems
- Pressure wounds
- Stroke
- Small risk of significant life-threatening event
General Risks of Spine Surgery
Although spine surgery is generally safe, there are some risks whenever operations on the spine are performed. These include:
- Infection 1-2%
- Bleeding. This can occur at the time of surgery and may necessitate a blood transfusion. It can also occur at some time after surgery. Rarely another operation is required to drain the bloodclot and stop the bleeding.
- Spine fluid leak (CSF leak)
- Small risk of significant neurological injury causing paralysis
- Chronic pain
Specific Risks of Transforaminal Lumbar Interbody Fusion
The specific risks will be discussed in detail prior to your surgery but may include:
- Pain in the lower back
- Nerve injury causing pain, numbness, weakness in the legs
- Nerve injury causing bowel or bladder problems
- Progressive deformity of the lumbar spine - kyphosis or spondylolisthesis
- Incomplete decompression of anterior pathology (unable to reach front of spine)
- Persistant symptoms
- Recurrence of symptoms
- Adjacent segment disease - problems at spine levels next to the fused level
- Non union - fusion not occurring
- Incorrect position of screws or other spinal implants
