Cervical Laminectomy
Cervical Canal Stenosis and Myelopathy Treatment
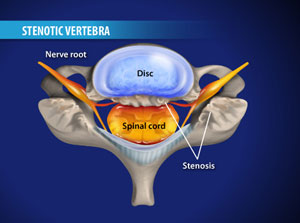
Cervical laminectomy is a very common and safe procedure that aims to relieve the pressure on the spinal cord and nerves in the cervical spine (neck). Most commonly it is performed to treat symptoms caused by cervical canal stenosis. This is a narrowing of the spinal canal that is caused by degeneration, or wear and tear, in the neck. Cervical stenosis and spondylosis can lead to conditions such as cervical myelopathy, brachialgia and cervical radiculopathy.
Spinal degeneration leads to the formation of bony overgrowths (spurs), arthritic joints, thickened ligaments and bulging discs, all of which can cause pressure on the spinal cord and nerve roots that go to your arms and hands. It is the pressure on the spinal cord and nerves that leads to symptoms such as:
- Pressure on the spinal cord causes cervical myelopathy
- Pressure on the cervical nerve roots causes brachialgia and cervical radiculopathy
Spinal degeneration leads to the formation of bony overgrowths (spurs), arthritic joints, thickened ligaments and bulging discs, all of which can cause pressure on the spinal cord and nerve roots that go to your arms and hands. It is the pressure on the spinal cord and nerves that leads to symptoms such as:
- pain in your arms (brachialgia)
- loss of feeling or numbness in your arms, hands and legs
- weakness in your arms, hands and legs
- difficulty walking
- gait disturbances
- difficulty performing fine motor movements
- neck pain
- bowel or bladder problems
|
Image showing compression on the spinal cord by cervical canal stenosis. A laminectomy "de-roofs" the spinal canal relieving pressure on the spinal cord and nerve roots..
 |
Following exhaustion of non-operative measures, or when the degree of spinal cord or nerve compression is severe, cervical laminectomy surgery is often indicated. Cervical laminectomy is performed under general anaesthesia. Patients are typically in hospital for between 2 and 5 days depending on how many levels need to be treated. Patients have a small incision in the midline at the back of the neck. The incision provides an excellent cosmetic result and is rarely noticed once the wound has healed. X-ray is used to accurately localise the correct levels. Sometimes more than one level may need to be treated by performing a laminectomy at multiple levels. |
Once the incision is made, muscle is retracted at the back of the spine to expose the bones of the spine. The bone at the back of the spine is called the lamina. The lamina "roofs in" the spinal canal that contains the spinal cord and the nerves which go to your arms. During a laminectomy, this bone is removed, thereby "de-roofing" the neural canal. Abnormal or overgrown ligament and bone spurs are removed to further relieve the pressure on the spinal cord and nerve roots.
Once the pressure on the nerves is relieved the wound is closed with absorbable sutures that don't need to be removed. The symptoms of arm pain are almost immediately improved. Weakness and numbness in the hands is usually slower to recovery. Neck pain is often worse in the immediate post operative period, however, slowly improves with time.
For the most part, cervical laminectomy is very safe surgery, however, there are some small risks. For more information about the risks of cervical laminectomy please see the information below in the risks of surgery section.
For more information about lumbar laminectomy watch the video below.
Once the pressure on the nerves is relieved the wound is closed with absorbable sutures that don't need to be removed. The symptoms of arm pain are almost immediately improved. Weakness and numbness in the hands is usually slower to recovery. Neck pain is often worse in the immediate post operative period, however, slowly improves with time.
For the most part, cervical laminectomy is very safe surgery, however, there are some small risks. For more information about the risks of cervical laminectomy please see the information below in the risks of surgery section.
For more information about lumbar laminectomy watch the video below.
Video demonstrating cervical laminectomy surgery
On some occasions performing a cervical laminectomy can lead to instability of the spine or progressive deformity. In these instances, Dr Oehme may advise fusing the cervical spine in addition to performing the laminectomy. This is called a posterior cervical fusion, or posterior lateral mass fusion. Spinal fusion is not performed routinely in spine surgery but may be needed where pain, instability or neurological problems may develop if the spine is not stabilised.
Spinal fusion involves stabilising a segment of the spine to allow bony union to occur across that segment, thereby immobilising that segment of the spine. Typically one or more spine levels are joined together to allow a bony bridge to form. The spinal segment to be fused is generally immobilised by the insertion of a rigid metal construct, such as lateral mass screws connected to rods.
Patients typically spend two to five days in hospital following cervical laminectomy. Following surgery walking is encouraged. Rehabilitation is sometimes needed, especially if more than one level has been treated or patients are elderly. Patients are advised to take things relatively easily for the first four weeks after surgery. Although patient's can walk and lift objects up to 5 kilograms, heavy lifting or prolonged bending is generally avoided. Patients can drive after one to two weeks. Pain relief in the postoperative period is easily controlled with oral pain medications.
Once the wound has healed after, usually after 7 days, hydrotherapy can be commenced. Physiotherapy can be started after 3-4 weeks.
Dr Oehme will advise if cervical laminectomy or posterior cervical fusion spine surgery is appropriate for your condition. For more information or to arrange a time to discuss surgery with Dr Oehme contact Keyhole Neurosurgery on 1800 DO SPINE (1800 367 746).
Risks of Cervical Laminectomy
Most cervical laminectomy surgeries can be performed safely without any complications. However, like any surgical procedure, there are risks associated with both the anaesthetic and the procedure itself.
Risks of Anaesthesia
Risks of anaesthesia will be discussed with you by your anaesthetist prior to surgery. It is important that you inform us of your correct age and any past medical problems, as this can influence the risk of anaesthesia. Risks include:
General Risks of Spine Surgery
Although spine surgery is generally safe, there are some risks whenever operations on the spine are performed. These include:
Specific Risks of Cervical Laminectomy
The specific risks will be discussed in detail prior to your surgery but may include:
Risks of Anaesthesia
Risks of anaesthesia will be discussed with you by your anaesthetist prior to surgery. It is important that you inform us of your correct age and any past medical problems, as this can influence the risk of anaesthesia. Risks include:
- Heart problems, such as heart attack (AMI) or arrhythmia
- Lung problems, such as infection (pneumonia) or blood clots
- Urinary tract infection
- Deep Venous Thrombosis (DVT)
- Eye or visual problems
- Pressure wounds
- Stroke
- Small risk of significant life-threatening event
General Risks of Spine Surgery
Although spine surgery is generally safe, there are some risks whenever operations on the spine are performed. These include:
- Infection 1-2%
- Bleeding. This can occur at the time of surgery and may necessitate a blood transfusion. It can also occur at some time after surgery. Rarely another operation is required to drain the bloodclot and stop the bleeding.
- Spine fluid leak (CSF leak)
- Small risk of significant neurological injury causing paralysis
- Chronic pain
Specific Risks of Cervical Laminectomy
The specific risks will be discussed in detail prior to your surgery but may include:
- Pain in the upper back and neck
- Nerve injury causing pain, numbness or weakness in the arm
- Spinal cord injury causing paralysis of the arms and legs
- Progressive deformity of the cervical spine - kyphosis
- Requirement for fusion at later stage
- Incomplete decompression of anterior pathology (unable to reach front of spine)
- Persistant symptoms
- Recurrence of symptoms
