Lumbar Canal Stenosis and Lumbar Spondylosis
Introduction
Lumbar spinal degeneration, or wearing out of the lumbar spine over time, can lead to what is called lumbar spondylosis and spinal stenosis. Lumbar spondylosis describes degenerative changes (arthritic changes) within the lumbar spine. Lumbar canal stenosis means narrowing or compression of the spinal nerves in the lower back due to spinal degeneration (wear and tear).
Introduction
Lumbar spinal degeneration, or wearing out of the lumbar spine over time, can lead to what is called lumbar spondylosis and spinal stenosis. Lumbar spondylosis describes degenerative changes (arthritic changes) within the lumbar spine. Lumbar canal stenosis means narrowing or compression of the spinal nerves in the lower back due to spinal degeneration (wear and tear).
|
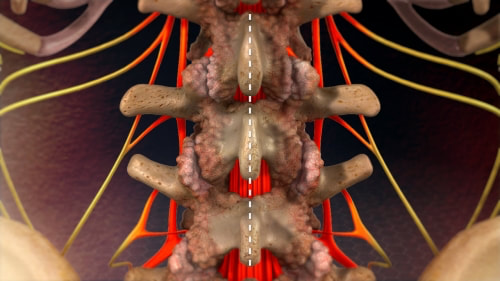
Image showing the lumbar spine with lumbar canal stenosis, prior to laminectomy. The nerves (red) are compressed by the overlying bone, or lamina.
|
Over time, spinal degeneration can lead to the formation of bony overgrowths (spurs), arthritic joints, thickened ligaments and bulging discs, all of which can cause narrowing (stenosis) around the nerves that go to your legs. It is abnormal pressure on spinal nerves that leads to symptoms such as pain in the legs (sciatica), numbness and tingling, weakness, difficulty walking and back pain. Laminectomy aims to improve these symptoms by relieving pressure on the spinal nerves. Watch the video below for more information about spinal stenosis. |
What is Spinal Stenosis
Disc degeneration at the affected level is thought to be the precipitating factor in spondylosis, with altered biomechanics resulting in abnormal loading and compensatory degenerative changes in other spinal structures(2). See our disc degeneration page for more information about intervertebral disc degeneration.
Lumbar canal stenosis and spondylosis are very common in the general population. It is rare to see in younger adults although it can occur. It more commonly occurs in the older population groups.
Lumbar canal stenosis and spondylosis are very common in the general population. It is rare to see in younger adults although it can occur. It more commonly occurs in the older population groups.
Symptoms of Lumbar Spondylosis and Lumbar Canal Stenosis
Lumbar spondylosis is a major cause of back pain, which commonly occurs due to concurrent degenerative disc disease or facet joint arthritis. In addition back pain can come from abnormal or stressed:
- Periosteum/bone
- Ligaments
- Paraspinal musculature and fascia
- Nerve roots
- Psychological causes
In addition to back pain, lumbar spondylosis is associated with symptoms of nerve compression which include:
- Leg pain (sciatica)
- Neurorgenic claudication (pain in backs of calves and legs with walking)
- Loss of feeling in the legs (numbness or parasthesias)
- Leg or foot weakness (for example foot drop)
- Problems with walking (gait disturbance)
- Troubles with bladder and bowel function.
Degeneration of the lumbar spine can lead to spinal nerve foramen narrowing (foraminal stenosis) causing nerve root compression and subsequent sciatica and radiculopathy. Radiculopathy is pain, numbness and weakness in the area that the nerve supplies.
Lumbar spondylosis can also lead to lumbar canal stenosis, or narrowing of the entire spinal canal at the affected level. Lumbar canal stenosis is narrowing or constriction of the central canal leading to compression of multiple nerves in the lumbar spine. Lumbar canal stenosis causes a syndrome known as neurogenic claudication, which is pain in the backs of the calves and legs, that is often worse with walking and standing and relieved by sitting down.
The symptoms of lumbar spondylosis are usually progressive and get worse with time. However, aith appropriate management the degree of progression can be slowed or even halted.
Investigations for Lumbar Spondylosis
Following the initial clinical assessment it is usual for some type of radiological investigation to be organised to look in more detail for the cause of the pain and discomfort and the degree of compression.
- MRI (Note if you are able to have an MRI, this is the best test to assess lumbar spondylosis and canal stenosis)
- CT
- X-ray
- Dynamic x-ray
- Bone scan including SPECT CT
Treatment options for spinal stenosis |
Surgery for lumbar spinal stenosis -
|
|
|
|
Treatment of Lumbar Spondylosis and Lumbar Canal Stenosis
Unless you have severe pain or significant neurological deficits, such as lower limb weakness, or bowel or bladder dysfunction, the initial treatments for lumbar spondylosis and lumbar canal stenosis are conservative non-operative therapies (3-5). These treatments include:
Following exhaustion of non-operative measures or when the degree of nerve compression is severe, surgery is often indicated for lumbar spondylosis. Where symptoms of nerve compression predominate, namely, radiculopathy or neurogenic claudication, the goal of intervention is to decompress the nerves, relieving the pressure on them. Relieving the pressure on the nerves reliably improves the symptoms of pain in the legs.
Classically a laminectomy with de-roofing of the neural canal is performed. In selected patients minimally invasive techniques will be appropriate and include, MIS laminectomy or more targeted lumbar decompression. If significant back pain exists, there is evidence of instability or spondylolisthesis, or the amount of decompression required is likely to cause instability, more complex fusion procedures are indicated.
80% of patients operated for lumbar spinal stenosis have good-to-excellent outcomes (6-8). Over 80% of patients are satisfied and report improvement in quality of life (8, 9). Decompressive surgery has been demonstrated to be superior to aggressive non-operative treatment in relieving symptoms and improving function(9, 10). For me information about surgery for lumbar spondylosis see our page on laminectomy, spine fusion and other spine surgery procedures.
References
1. Greenberg MS. Handbook of Neurosurgery. Sixth Edition ed: Thieme; 2006.
2. Latham JM. Mechanical consequences of annular tears and subsequent intervertebral disc degeneration. Clinical Biomechanics. 1994;9(July):211-9.
3. Kuijpers T, van Middelkoop M, Rubinstein SM, Ostelo R, Verhagen A, Koes BW, et al. A systematic review on the effectiveness of pharmacological interventions for chronic non-specific low-back pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2011;20(1):40-50.
4. van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2011;20(1):19-39.
5. White AP, Arnold PM, Norvell DC, Ecker E, Fehlings MG. Pharmacologic management of chronic low back pain: synthesis of the evidence. Spine. 2011;36(21 Suppl):S131-43.
6. Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine. 1992;17(1):1-8.
7. Airaksinen O, Herno A, Turunen V, Saari T, Suomlainen O. Surgical outcome of 438 patients treated surgically for lumbar spinal stenosis. Spine. 1997;22(19):2278-82.
8. Iguchi T, Kurihara A, Nakayama J, Sato K, Kurosaka M, Yamasaki K. Minimum 10-year outcome of decompressive laminectomy for degenerative lumbar spinal stenosis. Spine. 2000;25(14):1754-9.
9. Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, et al. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine. 1996;21(15):1787-94; discussion 94-5.
10. Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. The New England journal of medicine. 2008;358(8):794-810.
Unless you have severe pain or significant neurological deficits, such as lower limb weakness, or bowel or bladder dysfunction, the initial treatments for lumbar spondylosis and lumbar canal stenosis are conservative non-operative therapies (3-5). These treatments include:
- Analgesics (pain medication)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Physiotherapy
- Steroidal injection therapies
- Behaviour modification - e.g. avoiding heavy lifting
- Bracing
- Pilates
- Hydrotherapy
- Swimming
- Weight loss is also important as extra weight places more stress on the spine contributing to back pain.
- Exercises to strengthen core and paraspinal muscles will help provide extra stability to the spine reducing pain.
- Pain management
Following exhaustion of non-operative measures or when the degree of nerve compression is severe, surgery is often indicated for lumbar spondylosis. Where symptoms of nerve compression predominate, namely, radiculopathy or neurogenic claudication, the goal of intervention is to decompress the nerves, relieving the pressure on them. Relieving the pressure on the nerves reliably improves the symptoms of pain in the legs.
Classically a laminectomy with de-roofing of the neural canal is performed. In selected patients minimally invasive techniques will be appropriate and include, MIS laminectomy or more targeted lumbar decompression. If significant back pain exists, there is evidence of instability or spondylolisthesis, or the amount of decompression required is likely to cause instability, more complex fusion procedures are indicated.
80% of patients operated for lumbar spinal stenosis have good-to-excellent outcomes (6-8). Over 80% of patients are satisfied and report improvement in quality of life (8, 9). Decompressive surgery has been demonstrated to be superior to aggressive non-operative treatment in relieving symptoms and improving function(9, 10). For me information about surgery for lumbar spondylosis see our page on laminectomy, spine fusion and other spine surgery procedures.
References
1. Greenberg MS. Handbook of Neurosurgery. Sixth Edition ed: Thieme; 2006.
2. Latham JM. Mechanical consequences of annular tears and subsequent intervertebral disc degeneration. Clinical Biomechanics. 1994;9(July):211-9.
3. Kuijpers T, van Middelkoop M, Rubinstein SM, Ostelo R, Verhagen A, Koes BW, et al. A systematic review on the effectiveness of pharmacological interventions for chronic non-specific low-back pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2011;20(1):40-50.
4. van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2011;20(1):19-39.
5. White AP, Arnold PM, Norvell DC, Ecker E, Fehlings MG. Pharmacologic management of chronic low back pain: synthesis of the evidence. Spine. 2011;36(21 Suppl):S131-43.
6. Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine. 1992;17(1):1-8.
7. Airaksinen O, Herno A, Turunen V, Saari T, Suomlainen O. Surgical outcome of 438 patients treated surgically for lumbar spinal stenosis. Spine. 1997;22(19):2278-82.
8. Iguchi T, Kurihara A, Nakayama J, Sato K, Kurosaka M, Yamasaki K. Minimum 10-year outcome of decompressive laminectomy for degenerative lumbar spinal stenosis. Spine. 2000;25(14):1754-9.
9. Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, et al. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine. 1996;21(15):1787-94; discussion 94-5.
10. Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. The New England journal of medicine. 2008;358(8):794-810.