Laminectomy (Lumbar)
Lumbar laminectomy is a very common and safe procedure that aims to relieve the pressure on the nerves in the lower back (lumbar spine). It is most commonly performed to relieve the pain of lumbar stenosis and spondylosis. This is a narrowing of the spinal canal that is caused by degeneration, or wear and tear, in the lower back.
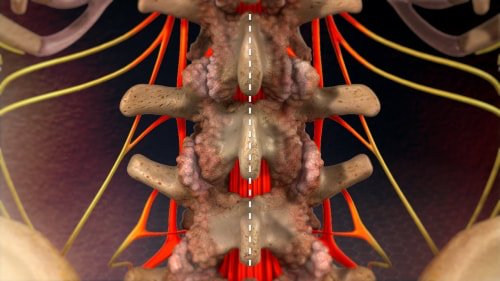
Spinal degeneration leads to the formation of bony overgrowths (spurs), arthritic joints, thickened ligaments and bulging discs, all of which can cause pressure on the nerve roots that go to your legs. It is the pressure on the nerves that leads to pain in the legs (sciatica), which is often worse with walking. When severe nerve compression is present weakness in the legs can occur that causes difficulty walking.
Lumbar laminectomy is a very common and safe procedure that aims to relieve the pressure on the nerves in the lower back (lumbar spine). It is most commonly performed to relieve the pain of lumbar stenosis and spondylosis. This is a narrowing of the spinal canal that is caused by degeneration, or wear and tear, in the lower back.
Spinal degeneration leads to the formation of bony overgrowths (spurs), arthritic joints, thickened ligaments and bulging discs, all of which can cause pressure on the nerve roots that go to your legs. It is the pressure on the nerves that leads to pain in the legs (sciatica), which is often worse with walking. When severe nerve compression is present weakness in the legs can occur that causes difficulty walking.
Following exhaustion of non-operative measures, or when the degree of nerve compression is severe, lumbar laminectomy surgery is often indicated for lumbar stenosis. Relieving the pressure on the nerves reliably improves the symptoms of leg pain in over 90% of patients.
Treatment Options for Lumbar Spinal Canal Stenosis |
Surgery For Lumbar Canal Stenosis -
|
|
|
|
Laminectomy is performed under general anaesthesia. Patients are typically in hospital for between 1 and 4 days depending on how many levels need to be treated. Where possible, Dr Oehme performs lumbar laminectomy using minimally invasive techniques.
Patients have a small incision in the midline of the lower part of their back. The incision provides an excellent cosmetic result and is rarely noticed once the wound has healed. X-ray is used to accurately localise the correct spinal level. The most commonly affected levels are L4-5 and L5-S1, however, other levels of the lumbar spine may also be affected by canal stenosis. Sometimes more than one level may need to be treated by performing a laminectomy at multiple spinallevels.
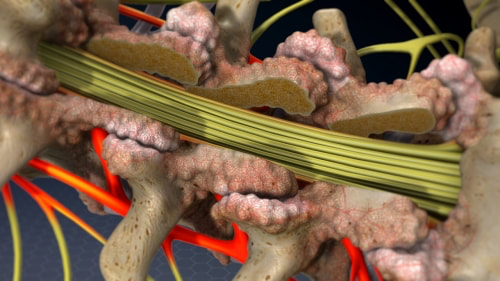
Once the incision is made, muscle is retracted at back of the spine to expose the bones of the spine. The bone at the back of the spine is called the lamina. The lamina roofs in the spinal canal that contains the nerves which go to your legs. During a laminectomy, this bone is removed, thereby "de-roofing" the neural canal. Abnormal or overgrown ligament and bone spurs are removed to further relieve the pressure on the nerves.
Patients have a small incision in the midline of the lower part of their back. The incision provides an excellent cosmetic result and is rarely noticed once the wound has healed. X-ray is used to accurately localise the correct spinal level. The most commonly affected levels are L4-5 and L5-S1, however, other levels of the lumbar spine may also be affected by canal stenosis. Sometimes more than one level may need to be treated by performing a laminectomy at multiple spinallevels.
Once the incision is made, muscle is retracted at back of the spine to expose the bones of the spine. The bone at the back of the spine is called the lamina. The lamina roofs in the spinal canal that contains the nerves which go to your legs. During a laminectomy, this bone is removed, thereby "de-roofing" the neural canal. Abnormal or overgrown ligament and bone spurs are removed to further relieve the pressure on the nerves.
|
Image showing the lumbar spine with lumbar canal stenosis, prior to laminectomy. The nerves (red) are compressed by the overlying bone, or lamina.
|
Image showing the lumbar spine following laminectomy. The lumbar nerves (yellow) are now longer compressed by the overlying bone, or lamina, which has been removed.
|
Once the pressure on the nerves is relieved the wound is closed with absorbable sutures that don't need to be removed. The symptoms of leg pain are almost immediately improved. Back pain is often worse in the immediate post operative period, however, slowly improves with time.
For the most part, laminectomy is very safe surgery, however, there are some small risks. For more information about the risks of lumbar laminectomy please sees the information below in the risks of surgery section.
For more information about lumbar laminectomy watch the video below.
For the most part, laminectomy is very safe surgery, however, there are some small risks. For more information about the risks of lumbar laminectomy please sees the information below in the risks of surgery section.
For more information about lumbar laminectomy watch the video below.
Video - Lumbar Laminectomy
Where possible, Dr Oehme performs lumbar laminectomy surgery using minimally invasive and keyhole techniques. This benefits patients by
Patients typically spend two to five days in hospital following laminectomy. Following surgery walking is encouraged. Rehabilitation is sometimes needed, especially if more than one level has been treated or patients are elderly. Patients are advised to take things relatively easily for the first four weeks after surgery. Although patient's can walk and lift objects up to 5 kilograms, heavy lifting or prolonged bending is generally avoided. Patients can drive after one to two weeks. Pain relief in the postoperative period is easily controlled with oral pain medications.
Once the wound has healed after, usually after 7 days, hydrotherapy can be commenced. Physiotherapy can be started after 3-4 weeks.
Dr Oehme will advise if lumbar laminectomy spine surgery is appropriate for your condition. For more information, or to arrange a time to discuss surgery with Dr Oehme, contact his rooms at contact@doneurosurgery.com, or 1800 DO SPINE (1800 367 746).
- minimising muscle injury
- reducing blood loss
- reducing infection risk
- reducing postoperative pain
- shortening the time spent in hospital
- utilising smaller more cosmetically favourable incisions
- reducing damage to adjacent levels
- reducing back pain
- reducing spinal instability
- preventing spondylolisthesis
Patients typically spend two to five days in hospital following laminectomy. Following surgery walking is encouraged. Rehabilitation is sometimes needed, especially if more than one level has been treated or patients are elderly. Patients are advised to take things relatively easily for the first four weeks after surgery. Although patient's can walk and lift objects up to 5 kilograms, heavy lifting or prolonged bending is generally avoided. Patients can drive after one to two weeks. Pain relief in the postoperative period is easily controlled with oral pain medications.
Once the wound has healed after, usually after 7 days, hydrotherapy can be commenced. Physiotherapy can be started after 3-4 weeks.
Dr Oehme will advise if lumbar laminectomy spine surgery is appropriate for your condition. For more information, or to arrange a time to discuss surgery with Dr Oehme, contact his rooms at contact@doneurosurgery.com, or 1800 DO SPINE (1800 367 746).
Risks of Lumbar Laminectomy
90% of patients operated for lumbar spinal stenosis have good-to-excellent outcomes. Over 80% of patients are satisfied and report improvement in quality of life. Most lumbar laminectomy surgeries can be performed safely without any complications. However, like any surgical procedure there are risks associated with both the anaesthetic and the procedure itself.
Risks of Anaesthesia
Risks of anaesthesia will be discussed with you by your anaesthetist prior to surgery. It is important that you inform us of your correct age and any past medical problems, as this can influence the risk of anaesthesia. Risks include:
General Risks of Spine Surgery
Although spine surgery is generally safe, there are some risks whenever operations on the spine are performed. These include:
Specific Risks of Lumbar Laminectomy
The specific risks will be discussed in detail prior to your surgery but may include:
Risks of Anaesthesia
Risks of anaesthesia will be discussed with you by your anaesthetist prior to surgery. It is important that you inform us of your correct age and any past medical problems, as this can influence the risk of anaesthesia. Risks include:
- Heart problems, such as heart attack (AMI) or arrhythmia
- Lung problems, such as infection (pneumonia) or blood clots
- Urinary tract infection
- Deep Venous Thrombosis (DVT)
- Eye or visual problems
- Pressure wounds
- Stroke
- Small risk of significant life-threatening event
General Risks of Spine Surgery
Although spine surgery is generally safe, there are some risks whenever operations on the spine are performed. These include:
- Infection 1-2%
- Bleeding. This can occur at the time of surgery and may necessitate a blood transfusion. It can also occur at some time after surgery. Rarely another operation is required to drain the bloodclot and stop the bleeding.
- Spine fluid leak (CSF leak)
- Small risk of significant neurological injury causing paralysis
- Chronic pain
Specific Risks of Lumbar Laminectomy
The specific risks will be discussed in detail prior to your surgery but may include:
- Pain in the lower back
- Nerve injury causing pain, numbness, weakness in the legs
- Nerve injury causing bowel or bladder problems
- Progressive deformity of the lumbar spine - kyphosis or spondylolisthesis
- Requirement for fusion at later stage
- Incomplete decompression of anterior pathology (unable to reach front of spine)
- Persistant symptoms
- Recurrence of symptoms
- Adjacent segment disease
Post-Operative Care & Instructions Following Lumbar Laminectomy
Post-Operative Care Following Lumbar Laminectomy (Lumbar Decompression)
The following information is provided to assist and maximise your recovery following your lumbar laminectomy, or lumbar decompression surgery.
If you have any questions or concerns not outlined below, please contact Dr Oehme’s rooms on 1800 367 746 (1800 DO SPINE), or contact@doneurosurgery.com, for further information.
The information provided below is general information for patients following lumbar laminectomy. Dr Oehme will explain any additional instructions which may be specific to you, or your operation, during your admission.
General Advise
Lumbar laminectomy, or lumbar decompression, is a procedure performed to alleviate symptoms of lumbar canal stenosis – compression of the nerves in the lower back due to spinal degeneration (wear and tear). It is usually performed to relieve symptoms such as sciatica (leg pain), difficulty walking, pins and needles, numbness or weakness in the legs and feet.
How much pain relief you will receive, and how quickly it will occur after lumbar laminectomy, is impossible to predict. Often patients will have immediate relief of their leg symptoms following the surgery. At other times, it may take weeks or months for symptoms to improve.
Some patients will have pain, numbness or weakness that does not completely improve and may be permanent. This is typically due to permanent nerve injury as a result of long-standing nerve compression from lumbar canal stenosis.
It is very common to have numbness and tingling in the legs and feet in the first few weeks after surgery. This slowly improves with time in most patients.
If you have had no improvement in your leg pain symptoms following the surgery, it is important to relay this to Dr Oehme.
It is very common to have back pain following a lumbar laminectomy. This is incisional and muscular pain and should slowly improve as the wound and muscles heal Any long-term chronic back pain you have had is unlikely to improve following a laminectomy.
It is important that you take things quietly for the first four to six weeks after surgery to let the wound heal and maximise your recovery.
During Your Hospital Stay
Most patients are in hospital for between one and four days following a lumbar laminectomy, after which they are usually discharged home. The more levels that are treated, the longer you will usually stay in hospital.
Most patients do not require inpatient rehabilitation following a laminectomy. It is recommended that a family member or friend drive you home from hospital.
If you are elderly, live alone, have had multiple levels treated, or are having problems with mobility, sometimes inpatient rehabilitation will be recommended. Inpatient rehabilitation aims to improve your strength, mobility and safety, prior to going home. If you require rehabilitation an ambulance will transfer you from the hospital to the rehabilitation facility.
To minimise the chances of infection you will typically have 24 hours of antibiotics following the operation.
Post-operative pain is generally well controlled with oral pain medications. It is important you ask for more pain relief if you feel your pain is not under control.
You will have stockings on your legs to prevent blood clots in the legs developing (DVT). You will also have calf compression devices fitted until you are mobile. Most patient also receive medication (Clexane) to prevent blood clots from forming.
Dr Oehme will review you during your hospital stay after your operation. You will then have a follow up appointment approximately four weeks after your discharge from hospital. A physician will also visit you to manage your pain and control any medical problems you may have.
Guidelines for Activities
Most patients can begin mobilising the day of surgery, or early the following day. Unless you are specifically told to remain in bed you can mobilise as soon as you have recovered from the anaesthetic.
The nurses and physiotherapists will help you sit out of bed. You can then progress to walking around the ward. It is important that you get up and walk around to prevent blood clots from developing in your legs and to maximise your recovery.
Walking: It is important that you start on a daily walking programme. Walking is the best exercise following surgery. Aim to be walking at least five times daily and slowly increase the distance you walk each day. Start with walking a small distance and slowly increase the distance each day. Patients who walk more have a much better recovery in the longer term.
Running: You should avoid running or jogging until Dr Oehme sees you at your post-op review and gives approval for more vigorous activities. Usually jogging can be commenced at six weeks following surgery.
Rest: Rest is also important to allow for healing. It is important that you rest, especially in the first two weeks following the surgery. It is best to rest in a lying down position.
Sitting: It is best to limit your sitting, especially if the surgery also involved removing a herniated disc. Typically, sitting should be restricted to one hour at a time to minimise the chance of recurrent disc prolapse. It is best to lie or stand, rather than sit, for long periods during the first four weeks after your surgery. It is important to have breaks if you are sitting for long periods of time. For example, if you are sitting at a desk you should aim to stand up and take a short walk once every hour.
Posture: Maintain a good posture. Stand up straight with your shoulders back. A sit-to-stand desk may be a good option for you if you are required to work at a computer or desk.
Lifting: No heavy lifting should be performed in the immediate post-operative period. You should not lift anything heavier than 5 kilograms for four weeks following surgery. At your four-week review Dr Oehme will usually increase the lifting limit.
Bending and Twisting: Minimise bending and twisting. Although you can bend and twist to perform necessary activities, such as putting your shoes and socks on, it is best not to perform any repetitive lifting, manual labour, or unnecessary bending and twisting.
Wound Care
Unless advised otherwise, your sutures will be dissolvable and will not need to be removed.
It is important that you keep your wound dry for one week following the surgery. You will be provided with waterproof dressings. You are able to shower with this dressing on. The dressing will need to be replaced following a shower, or when it is dirtied or soiled.
It is important not to have any restrictive clothing which is tight around the wound, or which rubs on the wound.
Any increasing wound pain or swelling, or any evidence of redness, heat, discharge, fluid leakage, wound breakdown or signs of infection, should be urgently reported to Dr Oehme's rooms or your local doctor.
After seven days, you can get the wound wet. It is best not to scrub or rub the wound in the shower. After two weeks, you are able to swim and get the wound completely immersed in water.
Medications
You will be discharged home on your normal medications and also some additional pain medications. Typically, after one week when your back pain is starting to settle, you can start to wean off your pain medications. It is important not to stop all the pain medications at once as this can lead to a recurrence of pain.
Lyrica: If you are taking Lyrica it should be weaned off slowly and should not be ceased abruptly.
Anticoagulation (Blood thinners): Typically, blood thinning medication (Plavix, Warfarin, Pradaxa, Xarelto, others) can be re-commenced one week (7 days) following surgery. Dr Oehme will discuss this with you during your hospital stay.
If you have any side effects from your medications, you can contact Dr Oehme's rooms or the nurses at the hospital. It is important that you inform Dr Oehme's rooms about any allergies that you might have.
Sitting and Working at a Desk
Always try and maintain a good sitting posture. Sit in a straight back chair with armrests. Do not sit in a reclining chair for the first four to six weeks after the surgery. Do not sit for periods longer than one hour. It is best to lie or stand rather than sit for long periods during the first four weeks of your recovery. If you are working at a desk, keep your computer screen and the reading material at eye level. You should consider getting a sit-to-stand up desk.
Lifting
You should not lift anything heavier than 5 kilograms for the first four to six weeks after surgery. You should abide by safe lifting practices and keep the load close to your chest. If you do need to lift something heavy, bend you knees and keep your back straight and minimise twisting and lifting.
Driving
You can drive after one week following a lumbar laminectomy if you feel up to it. There is no legal restriction preventing you from driving. If you have weakness in the leg, this should be discussed with Dr Oehme and you should consider whether driving is appropriate for you. In addition, if you are still taking strong medications, such as narcotics, you should not drive.
Physiotherapy
Physiotherapy, or other allied health input, is usually not required for the first four to six weeks after surgery. Dr Oehme will discuss commencing physiotherapy at your postoperative review at four weeks.
You may have been given some gentle exercises by the physiotherapist in hospital that you are able to perform. Although you can do these gentle exercises, aggressive physiotherapy is not required for the first four to six weeks after surgery. It is best if you focus on a walking programme. Once Dr Oehme has seen you at your postoperative review, he will give you clearance to pursue more aggressive physiotherapy or an outpatient rehabilitation programme.
Swimming and Hydrotherapy: Hydrotherapy and swimming can be commenced two weeks following the surgery as long as there have been no problems with wound healing.
Work:
Dr Oehme will discuss returning to work for you and this will depend on the job you perform. Typically, you will be off work for at least two weeks. If you perform a job involving manual labour or physical work, you may need to off work for up to four to six weeks.
Sports
Contact or competitive sports should not be played for three months following a lumbar laminectomy. Dr Oehme will discuss in detail about returning to sports at your four-week review.
Cleaning
Avoid vigorous cleaning and vacuuming until after your four-week review with Dr Oehme. Gardening or lawn mowing should also not be performed. Other jobs that require heavy lifting, or repetitive bending or twisting, should not be performed.
Bracing
You are not required to wear a brace following lumbar laminectomy surgery and Dr Oehme does not usually advise this.
Smoking, Alcohol and Illicit Drugs
Smoking, and excessive alcohol, will impede your recovery. If you smoke you will have a greater risk of poor wound healing, infection, complications in general, pneumonia, blood clots in the legs or lungs, all of which may necessitate further surgery.
Other Medical Symptoms
If you develop any of the following symptoms you should contact Dr Oehme’s rooms or your GP immediately:
- Raised temperature or fever
- Increasing leg pain, numbness or leg weakness
- Urinary or faecal incontinence
- Wound infection or breakdown
- Leg swelling
- Cough or shortness of breath
- Feeling generally unwell
If you develop chest pain, palpitations, extreme SOB or collapse, you should call “000” or present to the emergency department of your local hospital for assessment.
Follow Up
Unless there are any problems or you are advised otherwise, you will have a follow up appointment approximately four weeks following your surgery. This is generally the only appointment that is required following successful lumbar laminectomy surgery.
You should visit your GP one week following the surgery so that they can check your wound and write prescriptions for any pain medications you may need. If your GP has any concerns they can contact Dr Oehme directly.