Trigeminal Neuralgia
Information about Facial Pain and Trigeminal Neuralgia
|
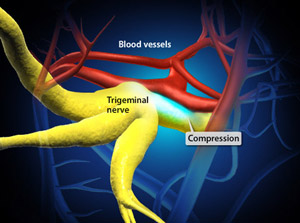
The trigeminal nerve (cranial nerve V) is a nerve that carries information about touch, pain and feeling from the face to the brain. Trigeminal Neuralgia is a chronic condition caused by a "mis-firing" of the trigeminal nerve. An attack causes brief episodes of extreme, shooting pain in one half of the face.
Often trigeminal neuralgia is due to compression of the nerve by a blood vessel in the brain. An MRI can sometimes demonstrate the blood vessel pressing on the nerve. In most cases trigeminal neuralgia can be managed with medication prescribed by a neurologist and no surgery is needed. |
 |
Sometimes, when symptoms become difficult to control with medication, surgery may be considered to treat the facial pain caused by trigeminal neuralgia. Surgery generally aims to move the compressive vessel away from the trigeminal nerve (microvascular decompression) and is successful in up to 90% of patients.
For more information about trigeminal neuralgia watch the video below or read about trigeminal neuralgia in more detail below.
For more information about trigeminal neuralgia watch the video below or read about trigeminal neuralgia in more detail below.
Video about Trigeminal Neuralgia
Trigeminal Neuralgia
Trigeminal neuralgia is a common facial pain syndrome. Patient’s with trigeminal neuralgia develop severe episodes of severe, lancinating facial pain. Although this condition is generally benign the pain can be quite debilitating and significantly impact on patient’s lives.
Trigeminal neuralgia is more common in females and 70% of patients with trigeminal neuralgia are over 50 years of age. Having said this, it is common to see trigeminal neuralgia in younger patients and in males patients.
Symptoms of Trigeminal Neuralgia
Trigeminal neuralgia is characterised by the sudden onset of severe, lancinating facial pain, lasting from a few seconds to less than a minute during episodes. It more frequently affects the lower part of the face and typically only occurs on one side of the face. The facial pain may be triggered by simple tactile stimuli such as light touch to the face, wind blowing on the face or chewing. In between painful episodes patients generally have pain-free intervals.
Patients with trigeminal neuralgia typically do not have any neurological deficits. Sometimes patients describe numbness or decreased sensation in the part of the face that is affected by the pain. If patients have underlying neurological deficits, such as cranial nerve palsies, it raises the suspicion for an underlying secondary cause of the trigeminal neuralgia.
Why do patients get trigeminal neuralgia?
Typical primary trigeminal neuralgia is said to be idiopathic, without any significant underlying cause. In these cases it is thought that vascular compression is the underlying cause. Rarely, trigeminal neuralgia can be caused by an underlying pathology such as a brain tumour or MS plaque (multiple sclerosis plaque). Routine MRI investigations rule out these more serious causes of trigeminal neuralgia, which have different treatment requirements.
The most common type of trigeminal neuralgia is the idiopathic type, and it is generally thought to be due to pressure on the trigeminal nerve from an aberrant loop of normal blood vessel in the brain. A blood vessel loop in in the brain, generally the superior cerebellar artery, presses on the entry zone of the trigeminal nerve to the brainstem causing the nerve to fire off sporadically, causing pain.
Most patients with classic trigeminal neuralgia have no clinical deficits. In cases due to tumour or MS there may be other focal neurological deficits. Some patients may have numbness in the face.
Investigation for trigeminal neuralgia are typically performed to exclude a more serious secondary causes for the trigeminal neuralgia. Investigations required are an MRI scan of the brain with contrast. There are also special MRI sequences including MRA and MRV, which aim to look for an aberrant vessel which is compressing on the trigeminal nerve. The superior cerebellar artery looping down and pressing on the root entry zone of the trigeminal nerve may be seen on MRI scan.
Treatment of Trigeminal Neuralgia:
The diagnosis and initial treatments for trigeminal neuralgia are typically administered by your GP or a neurologist.
Initial treatments for trigeminal neuralgia are to start with pharmacotherapy, also known as medical therapy. This typically involves treatment with a medication called Tegretol. A response to Tegretol is indicative of trigeminal neuralgia.
If pain persists following Tegretol, second-line pharmacotherapy may be instituted including medications such as Baclofen, Lyrica and Clonazepam.
If patient’s symptoms cannot be controlled with medication, then surgery is an option. Surgical options for treating trigeminal neuralgia include:
1. Microvascular decompression (MVD). In this procedure the aberrant vessel loop is moved away from the nerve. Watch the video below for more information about MVD for trigeminal neuralgia or see our microvascular decompression page for a detailed discussion about the surgery.
2. Percutaneous pain procedures. This include percutaneous procedure such as:
a) Radiofrequency ablation (RFA) of the trigeminal nerve
b) Glycerol injection of the trigeminal nerve.
c) Balloon compression of the trigeminal nerve.
3. Stereotactic radiosurgery (SRS) to the trigeminal nerve root entry zone. This focused form of radiotherapy can be used in cases that do not respond to other treatments.
Dr Oehme will discuss with the individual treatment options with you and recommend the best treatment for you. Factors such as your age, other medical problems, MRI findings and previous treatments all factor into the decision making process.
Most cases of trigeminal neuralgia is initially managed by neurologist. Following failure of medical therapy early referral to a neurosurgeon is important for consideration of surgery.
Trigeminal neuralgia is a common facial pain syndrome. Patient’s with trigeminal neuralgia develop severe episodes of severe, lancinating facial pain. Although this condition is generally benign the pain can be quite debilitating and significantly impact on patient’s lives.
Trigeminal neuralgia is more common in females and 70% of patients with trigeminal neuralgia are over 50 years of age. Having said this, it is common to see trigeminal neuralgia in younger patients and in males patients.
Symptoms of Trigeminal Neuralgia
Trigeminal neuralgia is characterised by the sudden onset of severe, lancinating facial pain, lasting from a few seconds to less than a minute during episodes. It more frequently affects the lower part of the face and typically only occurs on one side of the face. The facial pain may be triggered by simple tactile stimuli such as light touch to the face, wind blowing on the face or chewing. In between painful episodes patients generally have pain-free intervals.
Patients with trigeminal neuralgia typically do not have any neurological deficits. Sometimes patients describe numbness or decreased sensation in the part of the face that is affected by the pain. If patients have underlying neurological deficits, such as cranial nerve palsies, it raises the suspicion for an underlying secondary cause of the trigeminal neuralgia.
Why do patients get trigeminal neuralgia?
Typical primary trigeminal neuralgia is said to be idiopathic, without any significant underlying cause. In these cases it is thought that vascular compression is the underlying cause. Rarely, trigeminal neuralgia can be caused by an underlying pathology such as a brain tumour or MS plaque (multiple sclerosis plaque). Routine MRI investigations rule out these more serious causes of trigeminal neuralgia, which have different treatment requirements.
The most common type of trigeminal neuralgia is the idiopathic type, and it is generally thought to be due to pressure on the trigeminal nerve from an aberrant loop of normal blood vessel in the brain. A blood vessel loop in in the brain, generally the superior cerebellar artery, presses on the entry zone of the trigeminal nerve to the brainstem causing the nerve to fire off sporadically, causing pain.
Most patients with classic trigeminal neuralgia have no clinical deficits. In cases due to tumour or MS there may be other focal neurological deficits. Some patients may have numbness in the face.
Investigation for trigeminal neuralgia are typically performed to exclude a more serious secondary causes for the trigeminal neuralgia. Investigations required are an MRI scan of the brain with contrast. There are also special MRI sequences including MRA and MRV, which aim to look for an aberrant vessel which is compressing on the trigeminal nerve. The superior cerebellar artery looping down and pressing on the root entry zone of the trigeminal nerve may be seen on MRI scan.
Treatment of Trigeminal Neuralgia:
The diagnosis and initial treatments for trigeminal neuralgia are typically administered by your GP or a neurologist.
Initial treatments for trigeminal neuralgia are to start with pharmacotherapy, also known as medical therapy. This typically involves treatment with a medication called Tegretol. A response to Tegretol is indicative of trigeminal neuralgia.
If pain persists following Tegretol, second-line pharmacotherapy may be instituted including medications such as Baclofen, Lyrica and Clonazepam.
If patient’s symptoms cannot be controlled with medication, then surgery is an option. Surgical options for treating trigeminal neuralgia include:
1. Microvascular decompression (MVD). In this procedure the aberrant vessel loop is moved away from the nerve. Watch the video below for more information about MVD for trigeminal neuralgia or see our microvascular decompression page for a detailed discussion about the surgery.
2. Percutaneous pain procedures. This include percutaneous procedure such as:
a) Radiofrequency ablation (RFA) of the trigeminal nerve
b) Glycerol injection of the trigeminal nerve.
c) Balloon compression of the trigeminal nerve.
3. Stereotactic radiosurgery (SRS) to the trigeminal nerve root entry zone. This focused form of radiotherapy can be used in cases that do not respond to other treatments.
Dr Oehme will discuss with the individual treatment options with you and recommend the best treatment for you. Factors such as your age, other medical problems, MRI findings and previous treatments all factor into the decision making process.
Most cases of trigeminal neuralgia is initially managed by neurologist. Following failure of medical therapy early referral to a neurosurgeon is important for consideration of surgery.
Video - Microvascular Decompression for Trigeminal Neuralgia
This procedure eliminates (or greatly reduces) the sharp bursts of pain in the facial nerves caused by trigeminal neuralgia. The procedure is performed under general anesthesia and requires a short hospital stay.
