Sciatica & Lumbar Disc Herniation
|
|
|
|
|
|
Introduction
Sciatica is pain in the leg due to compression on a nerve in the spine. The pain is often like an electric shock going down the leg and can involve one or both legs. Sciatica is most commonly due to a disc herniation or prolapse compressing on a nerve in the lower spine. The pain can be severe and disabling, however, it is a common problem and easily managed by an experience neurosurgeon or spine surgeon. For more information watch the videos below.
In addition to pain, compression of a nerve can cause other problems in the area that the nerve supplies. This is called radiculopathy. Radiculopathy relates to dysfunction of a nerve root causing:
- Neurogenic pain (sciatica)
- Weakness of the foot or leg
- Reflex changes - such as loss of ankle jerk
- Sensory abnormalities (numbness and tingling) in the distribution of that nerve.
|
Commonly radiculopathy results from prolapse or herniation of a degenerative lumbar disc postero-laterally causing neural compression.
Less commonly, but more importantly, a large posterior disc herniation may cause cauda equina syndrome. This is where multiple nerve roots are severely compressed causing pain, leg weakness, urinary and bowel problems and anaesthesia around the buttock and genital area. If you have symptoms of cauda equine you should seek medical attention urgently at you local hospital. For more information watch the video below. |
|
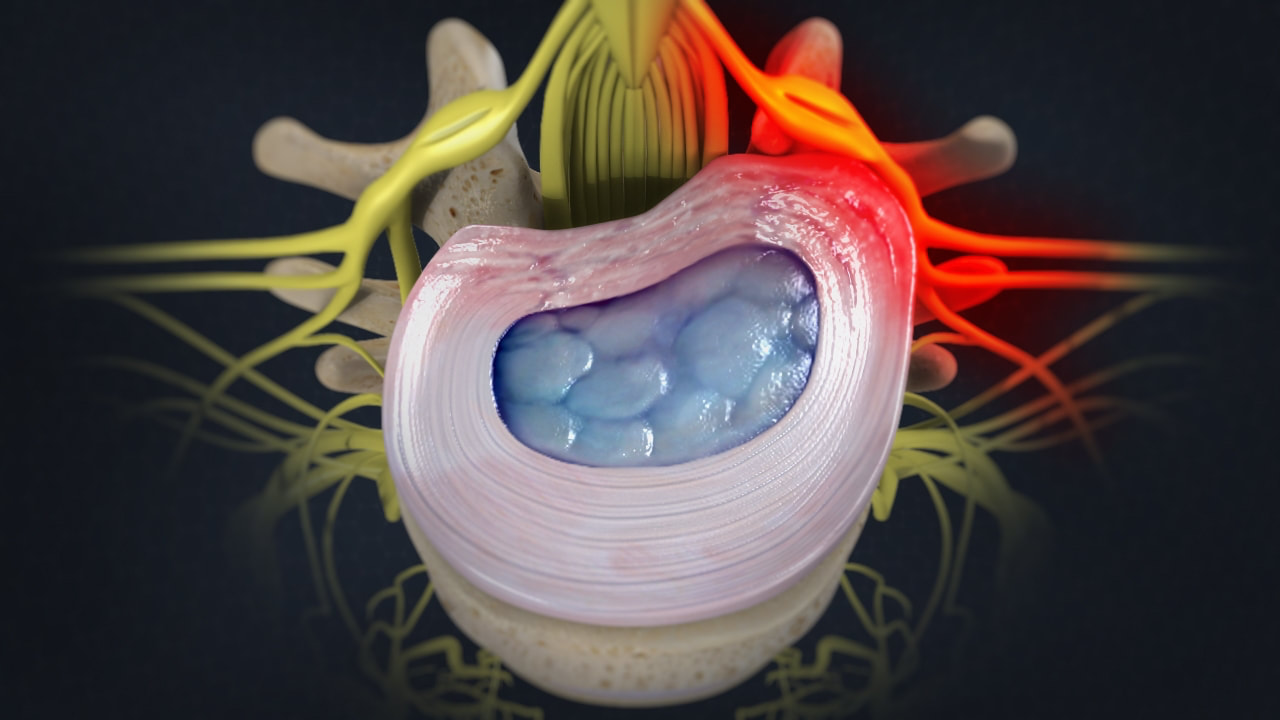
Image showing a lumbar disc herniation. The disc is compressing a nerve (red) which is inflamed. It is the nerve compression which causes the leg pain, or sciatica.
|
In addition to neurological compression from a degenerate, herniated or bulging disc, other abnormal structures in the vicinity of spinal nerves can cause compression. Lumbar spondylosis with combined ligament and facet joint overgrowth, as well as osteophyte formation (bony growth) or spondylolisthesis (slipping of one vertebrae on another), can contribute to compression of an exiting nerve root and subsequent radiculopathy(1).
Sciatica has a lifetime incidence of between 13-40% however up to 86% of episodes will resolve with aggressive non-operative therapies(2, 3). Small lumbar disc herniations are commonly seen on imaging in patients who are asymptomatic and do not require treatment(4). In addition, in patients with symptomatic disc prolapse, the majority of discs will regress over time without the need for surgical intervention(5). If the pain can be managed and there are no neurological deficits, often surgery can be avoided.
Conservative non-operative treatments are again the first line treatment for most patients with sciatica and disc prolapse. Behaviour modifications to avoid heavy lifting, sitting or weight bearing activities are usually recommended. In addition, the following therapies may be recommended:
These treatments include:
- Analgesics (pain medication)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Physiotherapy
- Steroidal injection therapies
- Behaviour modification - e.g. avoiding heavy lifting
- Bracing
- Pilates
- Hydrotherapy
- Swimming
- Weight loss is also important as extra weight places more stress on the spine contributing to back pain.
- Strengthening exercises to strengthen core and paraspinal muscles will help provide extra stability to the spine reducing pain.
- Pain management
In patients with lumbar disc prolapse, with pain or radiculopathy refractory to conservative therapies, decompressive surgery in the form of a microdiscectomy is indicated. In this procedure, a small unilateral laminotomy is performed followed by decompression of the compressed nerve root, by removal of the offending compressive fragment and a variable amount of disc tissue, the goal being to decompress the affected nerve and thus improve neurological symptoms. Up to 90% of patients will have improvement of sciatica and radiculopathy following microdiscectomy.
|
|
|